Introduction to Intestinal Parasites
Overview of Intestinal Parasites
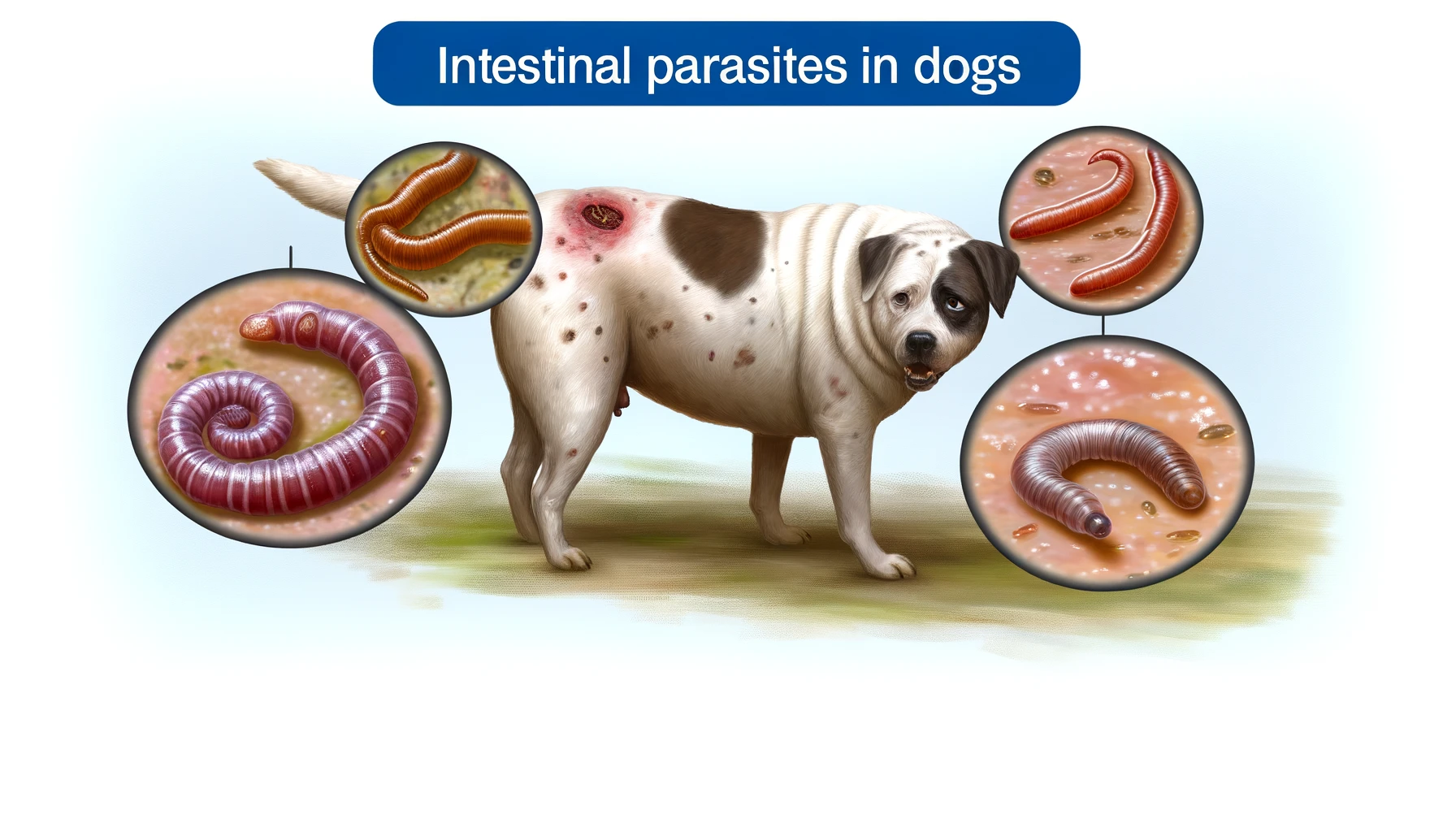
Intestinal Parasites, encompassing a variety of organisms such as roundworms, hookworms, and tapeworms, present significant health challenges worldwide. Intestinal parasites thrive in the gastrointestinal tract of humans, leading to infections that range from mild to severe, depending on the type of parasite and the overall health of the infected individual. Transmission routes are varied, often involving ingesting contaminated food or water, direct contact with contaminated soil, or, in some cases, through the bite of an infected insect. The burden of these infections is exceptionally high in regions with inadequate sanitation and hygiene practices. Symptoms of intestinal parasitic infections can include abdominal pain, diarrhea, malnutrition, and weight loss, though some infections may be asymptomatic. Given the wide range of parasites and the diverse ways in which they can infect humans, understanding the life cycle, transmission methods, and impact of these parasites is crucial for effective prevention and treatment strategies.
Common Types: Roundworms, Hookworms, Tapeworms
Roundworms, hookworms, and tapeworms are among the most prevalent intestinal parasites. Roundworms are typically ingested as eggs through contaminated food or water and can grow significantly within the intestines. Hookworms infect hosts through skin contact with contaminated soil, eventually reaching the intestines, where they feed on blood. Tapeworms are usually contracted by consuming undercooked meat containing larval cysts. Each type of parasite has a unique lifecycle and mode of transmission, contributing to different risk factors for infection. These include poor sanitation, lack of clean water, and practices such as eating undercooked meat or walking barefoot in contaminated areas. Awareness and understanding of these factors are essential for reducing the incidence of infections and promoting public health.
Transmission and Risk Factors
Intestinal parasites are primarily transmitted by ingesting contaminated food or water, contacting infected soil directly, or consuming undercooked meat from infected animals. Risk factors include poor sanitation, lack of clean water, living in or traveling to endemic areas, poor personal hygiene, and living in close quarters where infections can quickly spread. Children, in particular, are at higher risk due to their tendency to play in the dirt and put objects in their mouths, making them more susceptible to ingesting parasite eggs. Preventative measures, including improving sanitation, practicing good hygiene, and ensuring proper food cooking, are crucial in mitigating the risk of infection.
I believe this is among the so much important info for me. And i’m glad studying your article. But wanna remark on some normal issues, The web site taste is ideal, the articles is in reality excellent : D. Just right activity, cheers